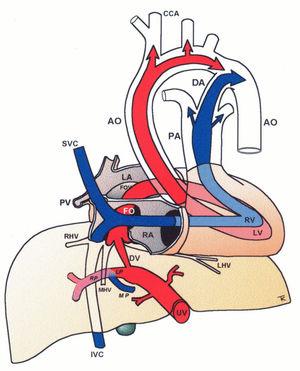
While biometry and Doppler have proved useful in the management of fetal growth restriction, the same battery has been of less help in diabetic pregnancies. It is not surprising since the underlying pathophysiology is fundamentally different. Recent studies of the fetal liver, a key metabolic organ, have shown that its venous circulation reflects the impact of maternal hyperglycemia. Umbilical return from the placenta is disproportionately distributed to the fetal liver (more than in normally growing fetuses, and more than in non-diabetic macrosomia). However, what is set as a pattern at midtrimester is not followed up in the 3rd trimester when high fetal growth continues but no longer correspondingly supported by the umbilical flow to the liver (mLmin−1kg−1 is low). Thus, the status at 3rd trimester is as follows: umbilical flow does not match fetal growth, but the fetal liver still takes a major proportion of the placental return leaving less for the ductus venosus (DV). A distended DV does not help; rather it indicates reduced residual compensatory mechanisms to face hypoxic challenges.
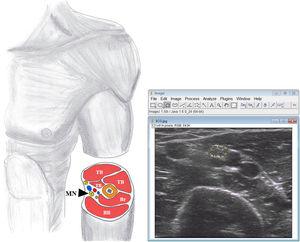
The new insights suggest taking into consideration the fetal liver when assessing risks in diabetic pregnancies at 3rd trimester. Measuring umbilical venous flow and its distribution requires high level of skills and accurate techniques, but in the left portal branch (between the DV inlet and the junction with the portal main stem), the blood velocity is regularly accessible and it reflects the skewed umbilical flow to the liver, and its consequences, in a graded manner.