Background
Patients with chronic spontaneous urticaria frequently relapse after discontinuing omalizumab and require its reintroduction. Although prior optimization might reduce recurrences, there is scarce evidence on this issue. Moreover, predictors of relapse have been identified in non-optimized patients before suspension.
Methods
We conducted a multicenter retrospective study with patients who discontinued omalizumab after optimization with a 12-month follow-up. Univariate and multivariate (tree classification method and Cox regression) analyses were performed.
Results
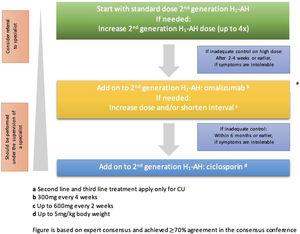
A total of 131 patients were included, 32.8% of whom relapsed after 12 months. Relapsed patients had longer disease duration (24.00 vs 11.00 months; p=0.032), quicker response to standard dosage (1.00 vs. 3.00 months; p=0.014), fewer complete responses pre-optimization (83.70% vs 95.50%; p=0.023), and shorter treatment duration at 300mg/4 weeks (6 vs 7 months; p=0.035). Multivariate analysis revealed that patients with low baseline C-reactive protein (CRP) and total immunoglobulin E (IgE) who underwent prolonged treatment were more likely to maintain a sustained remission at 12 months.
Conclusion
Optimization seems to reduce the relapse rate after discontinuation. The most relevant factors for recurrence are associated with the duration of treatment at different doses of omalizumab, along with the baseline CRP and total IgE levels. To minimize relapse after suspension, a 12-month treatment regimen at 300mg/4 weeks followed by an 18-month dose tapering is proposed.