Objective
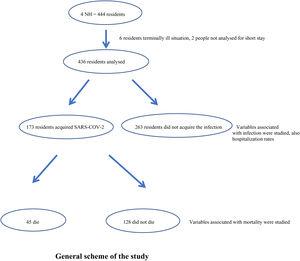
The aim of this paper was to analyse the association of demographic, clinical and pharmacological risk factors with the presence of SARS-COV-2 virus infection, as well as to know the variables related to mortality from COVID-19 in nursing home (NH) residents.
Design
Retrospective case–control study. The study variables of those residents who acquired the infection (case) were compared with those of the residents who did not acquire it (control). A subgroup analysis was carried out to study those variables related to mortality.
Site
Nursing homes in the region of Guipúzcoa (Spain).
Participants and interventions
4 NHs with outbreaks of SARS-CoV-2 between March and December 2020 participated in the study. The infectivity and, secondary, mortality was studied, as well as demographic, clinical and pharmacological variables associated with them. Data were collected from the computerised clinical records.
Main measurements
Infection and mortality rate. Risk factors associated with infection and mortality.
Results
436 residents were studied (median age 87 years (IQR 11)), 173 acquired SARS-CoV-2 (39.7%). People with dementia and Global Deterioration Scale ≥6 were less likely to be infected by SARS-CoV-2 virus [OR=0.65 (95% CI 0.43–0.97; p<.05)]. Overall case fatality rate was 10.3% (a mortality of 26% among those who acquired the infection). COVID-19 mortality was significantly associated with a Global Deterioration Scale ≥6 (OR=4.9 (95% CI 1.5–16.1)), COPD diagnosis (OR=7.8 (95% CI 1.9–31.3)) and antipsychotic use (OR=3.1 (95% CI 1.0–9.0)).
Conclusions
Advanced dementia has been associated with less risk of SARS-CoV-2 infection but higher risk of COVID-19 mortality. COPD and chronic use of antipsychotics have also been associated with mortality. These results highlight the importance of determining the stage of diseases such as dementia as well as maintaining some caution in the use of some drugs such as antipsychotics.