Introduction
The prevalence of COPD phenotypes that are referred for assessment for lung transplantation is unknown, as well as whether specific phenotype influences post-transplant evolution in those patients who receive it.
Material and methods
Ambispective observational study without intervention. The main objective was to know the prevalence of the different COPD phenotypes of the patients referred for the evaluation of a lung transplant. Secondary objective were to compare their clinical characteristics, to perform an analysis of post-transplant survival or complications according to their phenotype.
Results
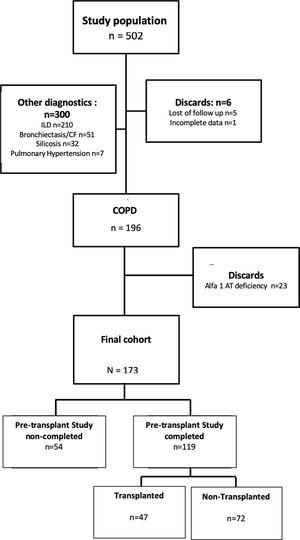
502 patients were evaluated for lung transplantation, of which 173 met the study criteria. 31.21% of the patients were discarded for transplantation on a first visit. The final cohort of potential transplant candidates who completed the pre-transplant study was 119 (69%) and 47 finally received a lung transplant (39.5%). The most frequent COPD phenotype evaluated for lung transplantation was the exacerbator (59%), followed by the non-exacerbator (38%) and the Asthma COPD Overlap [ACO] (3%). 59.8% of the exacerbator-phenotype patients assessed did not complete the pre-transplant study. Exacerbator-phenotype patients have a lower post-transplant survival (1115.1 days [standard deviation-DE-587]) vs. ACO: 1432 days [DE 507.5] and Non-exacerbators: 1317.8 days [DE 544.7] p=0.16), although this difference has not been statistically significant.
Conclusions
The most frequent COPD phenotype assessed for lung transplantation is the exacerbator, although more than half of these patients fail to complete the pre-transplant study.