Introduction
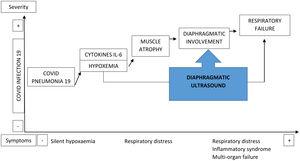
COVID-19 pneumonia results in an impairment of the diaphragmatic musculature that influences the development of respiratory failure during the patient's hospitalization. Diaphragmatic ultrasound is a useful, non-invasive, and accessible tool for measuring the function of this muscle.
Objective
Assessing the morphological and functional ultrasound status of the diaphragm in patients admitted within the first 24h for COVID-related pneumonia and its association with hospital morbidity and mortality (NCT05805579).
Material and methods
Observational, prospective cohort study that included 68 patients admitted for COVID-19 pneumonia with respiratory failure. Diaphragmatic ultrasound was performed within the first 24h of admission to the pulmonology ward. Clinical, analytical, and ultrasound variables were collected: excursion, thickness, and diaphragmatic shortening fraction (DSF). DSF<20% was used to define diaphragmatic dysfunction (DD). Patients who showed favorable progression and were managed on the ward (HCONV) were compared to those who required admission to the respiratory monitoring unit (RMU).
Results
A total of 68 patients were included, of which 22 (32.35%) were admitted to the RMU. Diaphragmatic excursion at maximum volume was higher in the HCONV group compared to the RMU group (58.41±17.83 vs. 50.03±16.23; p=0.123). Diaphragmatic dysfunction (DD) was observed in 21 (30.88%) patients, with a higher prevalence in the RMU group than in the HCONV group (15 (68.18%) vs. 6 (13.04%); p=0.0001). In the multivariate analysis, age and DSF at admission were the best predictors of failure to discharge.
Conclusions
Performing diaphragmatic ultrasound to assess mobility and DSF within the first 24h of admission for COVID-19 pneumonia proves valuable in determining short-term progression and the need for admission to a respiratory monitoring unit.