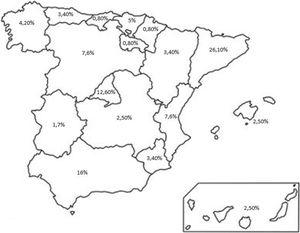
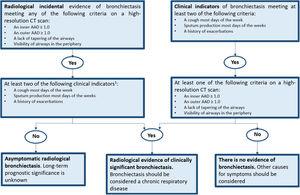
Pulmonary nocardiosis is a rare opportunistic infection, often misdiagnosed due to its subacute onset and non-specific clinical and radiological findings. We report an 82-year-old man with severe chronic obstructive pulmonary disease (COPD) and bilateral bronchiectasis, who presented with progressive dyspnoea and productive cough unresponsive to conventional antibiotic therapy. Nocardia pneumoniae was isolated from bronchoalveolar lavage at ≥104CFU/mL. Initial treatment with trimethoprim–sulfamethoxazole (TMP–SMX) was discontinued due to renal impairment and electrolyte disturbances; minocycline was initiated with good tolerance and complete radiological resolution after six months. This case highlights the need to suspect nocardiosis in COPD and bronchiectasis patients, even without classical immunosuppression, particularly after repeated corticosteroid courses. Early diagnosis, communication with the microbiology laboratory, and targeted antibiotic therapy are key to improving outcomes.