Background
Despite progresses in autoimmune encephalitis and related disorders (AERD), they remain a major challenge in daily clinical practice.
Objectives
To describe a tertiary hospital's longitudinal experience in AERD between 2005 and 2020.
Methods
Single-centre retrospective analysis of 43 patients.
Results
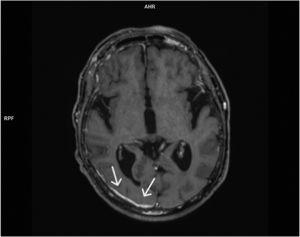
43 patients were included, 55.8% with positive antibodies (10 antiGAD, 4 antiNMDAR, 2 antiGABABR, 2 antiLGI1, 2 antiCASPR2, 1 antiIgLON5, 1 antiHu, 1 antiYo, 1 antiCV2 and 1 antiMa2, detecting coexisting antibodies in one patient: antiNMDAR+antiGABABR); 28% with negative antibodies; and 16.2% with steroid responsive encephalitis associated to antithyroid antibodies (SREAT). The median age was 62 years-old [14–88]. Females (62.8%) outnumbered males (37.2%). Limbic encephalitis was the most common clinical syndrome (60.5%), followed by SREAT (16.2%), autoimmune cerebellitis (9.3%), stiff-person syndrome (7%), antiNMDAR-encephalitis (5%) and antiIgLON5 encephalopathy (2%). CSF showed pleocytosis and/or hyperproteinorrhachia in 54.2%. MRI was unremarkable in 60%. Brain SPECT/PET showed hyperperfusion/hypermetabolism of limbic areas in 60% of patients to whom it was performed. Antibody-positivity was significantly associated with satisfaction of diagnostic criteria at high levels of certainty (p < 0.001). Treatment escalation was more frequent in antibody-positive patients. The creation of a Neuroimmunology Unit improved diagnostic and treatment approaches.
Conclusions
AERD's diagnosis and treatment have significantly improved over the last years. However, several limitations remain, particularly concerning antibody-negative AERD. The proposed diagnostic criteria might be still too reliant on antibody-positivity. Antibody-status seems to condition treatment escalation. The creation of a Neuroimmunology Unit optimized AERD's management in clinical practice.